Web 2.0 and Employee Engagement
in Next-Generation Healthcare Consumerism
Participatory information technology platforms can enhance the effectiveness of next generation Healthcare Consumerism. New Health Advocacy Program (HAP) strategies use various participatory Web-based approaches—aimed to engage end-users and accelerate behavior change. Innovative Web 2.0 aggregator/navigator platforms can engage participants to optimize Healthcare Consumerism savings of 9-21% and separately provide additional value-added savings of 2-4%. Web 2.0 and next generation “Health Advocacy Programs (HAPs)” can enhance financial successes as well as achieve better participant engagement and overall satisfaction.
-
Introduction
Healthcare Consumerism comprises the next generation of Consumer-Directed Health Plans (CDHP’s): it is about transforming an employer’s health benefit plan into one that puts economic purchasing power—and decision-making empowerment—into the hands of end-user participants. It’s also about supplying the information and decision support tools that they need, along with financial incentives, rewards, and other benefits that encourage personal involvement in altering health and healthcare purchasing behaviors.
Building a new generation health plan is, therefore, much more than employers merely implementing high deductible plans with attached health saving accounts. Those 1stgeneration plans tend to generate savings from discretionary spending (prescription drugs, office visits, emergency room use, and some diagnostic/x-ray/lab expenses). Arguably, a large portion of early-stage CDHP results can be attributed to cost-shifting and other anomalous new-program induction effects. Next generation plans, however, must provide greater levels of support and participant engagement in order to sustain ongoing behavior changes and savings. Innovative information aggregation/navigation and social networking (a.k.a.,Web 2.0) methods offer a promising new stimulant for establishing successful CDHP programs.

1st Generation Consumerism- Focus on high deductible plan designs, implementation of personal care accounts (HRAs, HSAs, FSAs), and basic decision support tools. Impact: Discretionary Expenses.
2nd Generation Consumerism- Focus on behavior changes and the use of all plan designs with individual and group incentives/rewards to effectively change health and healthcare purchasing behaviors. Impact: Chronic & Persistent Conditions, Pre-Natal, Wellness & Preventive care.
3rd Generation Consumerism- Focus on health and organizational performance and the integration with how consumerism and behavior change affects work performance and the corporate bottom line. Impact: Organizational health, turnover, absenteeism, productivity, disability, presenteeism, unscheduled sick days, creativity, and teaming.
4th Generation Consumerism- Focus on lifestyle, lifecycles, personal health needs, and the impact of how behavior change affects personal health and healthcare. Impact: Lifecycle needs, personal health, genetic predispositions, predictive modelling, healthy habits, and wellness.
The core value of an effective aggregator/navigator will include ways and means to support employer health plans as they evolve through the multiple generations of change. Today, most employers and product vendors are focused on implementing 2ndgeneration healthcare consumerism strategies. But the process of truly engaging plan members and optimizing on the promise of healthcare consumerism is a multi-year/multi-generation effort that requires tools and capabilities to assist members with simple user-friendly interactions.
The future is about empowering individuals with information to foster confidence in assuming ever-higher reaches of personal responsibility. It’s about supporting healthy behaviors and engaging employees in a new set of relationships that deal with maximizing their “human capital health” rather than just financing sickness and disease. In short, a platform that provides these kinds of support functions is instrumental to next generation CDHP programs.
-
The Multi-program/Multi-generational Navigator/Aggregator Opportunity
Today’s CDHPparticipants are faced with an assortment of disconnected programs, all aimed to effect one kind of behavioral change or another. Multiple vendors are involved, complicated tools are often available, and variously helpful resources offered. But, these disjointed tools too often only add to the already confusing world of healthcare.
In other words, many employers are implementing numerous wellness and disease management programs—perceivably, just to lower their overall healthcare costs. Ideally these programs would be proactively organized programs providing lifestyle support and they would offer medical/clinical assistance to employees and their family members in maintaining their health.
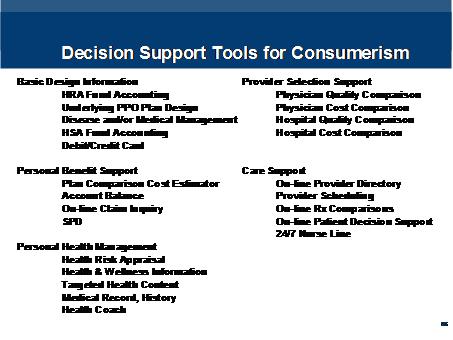
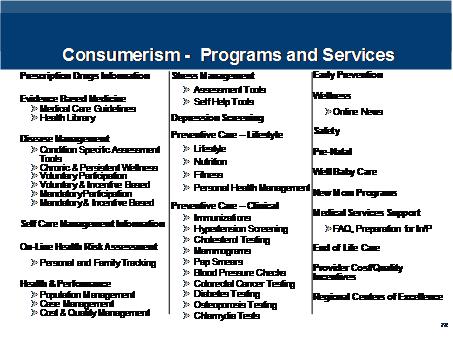
Plan members are easily overwhelmed with so many consumerism decision support tools, programs, and services. HoIP, developed by DCS, is an example of a platform to connect, simplify and organize plan offerings. Technologies such as HoIP simplify and cut through the maze of program complexity, minimizes information overload, and moderates the anxiety of the ignorance. The following discussion of Web 2.0 platforms and their potential to impact next generation Healthcare Consumerism will use HoIP as an example.
III. The Web 2.0
One of the most astonishing developments in history involves the cascading scope, scale and speed in which the internet is transforming global education, entertainment, commerce, etc; and, at last, it’s now knocking on healthcare’s door as well. There are two relevant phases of internet development important in the use of Web 2.0 with healthcare: (1) the emergence of the world wide web—as the increasingly dominant means by which consumers request and retrieve information; and, (2) the more recent phenomena of explosive two-way interactive communications and user-generated-content (UGC)—as the means by which passive consumption is transformed toactive participation.
Often referred to collectively as Web 2.0, this expanding collection of social networking, Wikis, BLOG/VLOG’s and other participatory applications is transforming both the nature and volume of internet traffic in startling proportions!
Inasmuch as healthcare consumerism’s ultimate success turns upon end-user behavior change and, inasmuch as behavior change turns upon active engagement and regular participation, effective communication (of expanding options) and incentives (to exploit them) are key. Thus presupposing that, in fact, the more participatory impacts of Web 2.0 will impact healthcare at even the fraction of that being experienced in other industries, the results will be to move the CDHP savings potential needle yet higher than previously anticipated.
A Web 2.0 information platform promises to increase participation and, therefore, lift overall saving potential in three ways: faster individual discovery and adoption; more individuals electing to avail themselves of next-generation CDHP programs; and better more faithful adherence to CDHP/HAP’s various opportunities.
IV. Navigating Information
Just as the best things in life are free, the best tools are the ones that make a hard, or complex, job seem simple. And, paradoxically, the tools that seem simplest, on their surface, are the most complex inside: the new Apple iPhone, for example, contains an order of magnitude more code than the previous market-leading Motorola Razr. Moreover, inasmuch as most users have some familiarity with conventional internet tools, those skills can be repurposed within a multi-pane window: i.e., into targeted services, search engines, messaging, social networking and other new Web 2.0 interfaces.
A distribution of typical health claims shows a spectrum of risk factors where each segment may require targeted solutions. A plan member may find that in any given year that they fall into several segments. It follows then, that just as the kind of information that they may want/need will vary, the best method of bi-directionally communicating it will too. In other words, the best way to “navigate” an end-user to the best source, from an explosive array of web sites, will involve a synergistic set of new information tools.
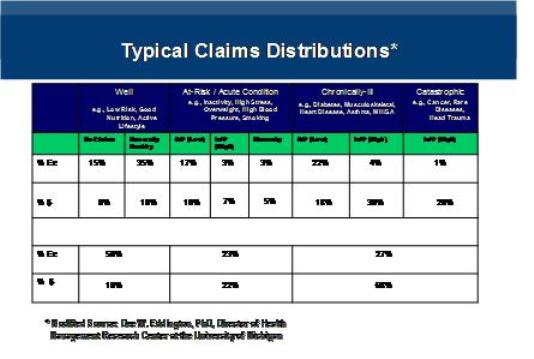
Plan members who are “low risk” need to stay “well” through prevention. The “at-risk” population needs early intervention, and lifestyle wellness education. The “high risk” and chronically ill population needs help in stabilizing their condition and understanding treatment options and the benefits of compliance in minimizing complications and costs.
Web 2.0 platforms intelligently direct and guide individuals to information, plan services, like individuals, and more promising sources for the answers to their instant questions. It may also help plan members navigate plan information, web-based resources, and on-line community support groups to affect the behavioral change impact points.
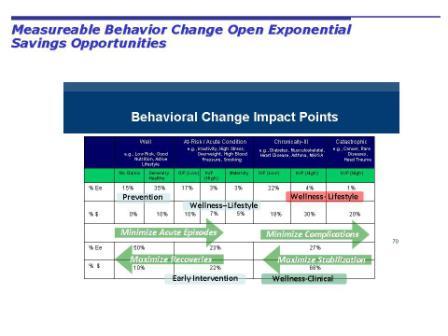
Lowering costs requires real behavioral change: an effective healthcare consumerism program requires active engagement of individuals and patients in the complex world of health, healthcare, and health insurance. A Web 2.0 platform encourages real behavior change through meaningful information and support links for medical, clinical, and lifestyle decisions.
An example of such a broad array of information navigation and cyber-health would do the following:
-
Contextual Based Inference and Advocacy – continuously capture the context of the operations being performed (e.g., searching for information on diabetes) and uses that information to provide supportive guidance, or advocacy, making the user’s experience faster, easier, and more efficient.
-
MyCommunities – A powerful source of behavior support through social networking. Utilizing the HoIP intelligent search engine (called The Rover), MyCommunities connects users to a broad array of blogs and message boards related to areas of interest, or context, they’re currently pursuing.
-
MyHealth– Users are able to find, update, and interact with all of their health related information, plans, and services. Users are guided through the complex array of health plan information by our system’s ability to detect the context of the user’s area of interest.
-
MyWeb– Users are empowered to more efficiently and effectively search the web for information via our combination of the latest generic and health related search engines operating within the context of the specific health subject of interest being pursued.
-
MyMessages– Users are able to interact with others without leaving the HoIP-enhanced Portal by employing the messaging capabilities extant in our MyMessages service.
Web 2.0 technology provides simplified identification, location, communication and transference of individual-centered health and healthcare information; thus, it provides a unique nexus of web-based links, health communities, interaction with similarly situated individuals, and insurance plan coverage information.
-
Aggregating Information
Some “next generation” CDHP initiatives and Health Advocacy Programs are already underway; others are in active development and implementation and/or on the drawing boards.

With so much information to overwhelm plan members, a single aggregator/navigator of internal and external resources is critical. Moreover, an open platform, that reaches across the entire internet and opens up a wider world of reliable information, can establish user trust that options and choices are being presented. Employees are suspicious of limited choices where vendors direct patients to their products and solutions.
Web 2.0 platforms can be completely open or narrowed to credentialed information. Alternatively, some sponsors may prefer to position/brand the aggregator/navigator tools as entirely neutral. But, in most cases, the opportunity to more properly subordinate, and synergistically integrate, the collective power of a plan’s “virtually confederated vendors” brings benefits to all.

As an example, the above platform allows for aggregating information and integrating a suite of next generation wellness programs. Its various “parallel paths” through the internet also provide a more economical, dynamic and flexible super-portal gateway architecture.
VI. Measuring Healthcare Consumerism Savings Potential
The Center for Disease Control studies show that 50% of health status is behavioral. To lower these plan costs requires increased individual personal responsibility that is the hallmark of healthcare consumerism. Once again, active participation is the key.

Other reputable studies corroborate these findings. The often referenced Rand Health Insurance Experiment (HIE), for example, proved that 45% of health expenditures are not driven by need, but because someone else paying the bill.
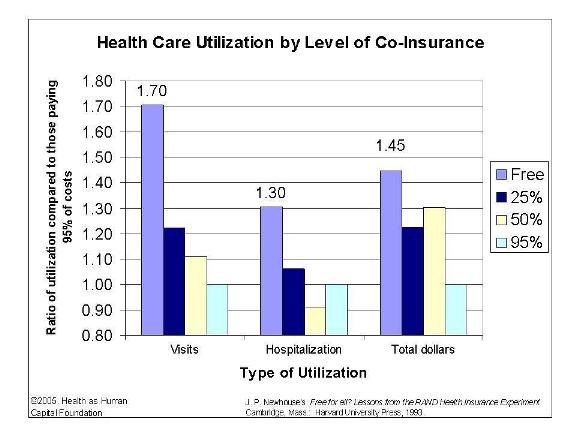
This would seem to imply that next-generation cost savings, healthcare consumerism will work only if plan members are empowered with information and resources to change behaviors. The Chart below shows the potential savings of 9% to 21% based upon modest and major changes to health status for a given population.

From this potential level of healthcare consumerism savings, the challenge is to unlock the behavior savings and the power of engaging plan members and patients with personal responsibility. Starting from a foundation for potential next generation CDHP savings, the following breaks the problem two parts: first, it lays out a range of next-generation CDHP/HAP savings; form there, reasonable assertions are made about how an effective aggregator/navigator can accelerate if not improve upon these savings ranges of 9% to 21%.
Web 2.0 platforms can interactively engage employees with state-of-the art intelligent search and retrieval processes that provide informative links, health condition social networking and interactive messaging – all with the ability to relate wellness, prevention, treatment, and cure options to their existing plans of coverage. Within (and beyond) these CDHP/HAP opportunity ranges, there are three generic opportunities to “enhanced” value:
-
Faster: earlier participant adoption (and accelerated savings)
-
More: participants adopting HAP programs (and more savings)
-
Better: participant adherence (better results and savings)
VII. Toward Quantifying the Overall Value
The need for wellness and other HAP programs is clear. It is the right effort for employers to move employees towards next generation healthcare consumerism. For every 100 members:
1. 29% have high blood pressure 7. 30% have cardiovascular disease
2. 80% do not exercise regularly 8. 55% or more are overweight or obese
3. 6-9% have diabetes 9. 10% are depressed
4. 35% are under significant stress 10. 50% do not wear their seat belts
5. 23-30% smoke (70% want to quit, 35% try each year)
6. 30% are prone to low back pain (many linked to obesity)
The challenge is how to best organize, aggregate, and navigate the many potentially beneficial programs and initiatives. Without a solid platform from which to build future generation healthcare consumerism, the multitude of programs, services, and tools will only further confuse patients.
A Web 2.0 platform can provide the foundation for plan evolution into next generation healthcare consumerism with potential savings of 9-21%. A supporting aggregator/navigator platform is critical to creating and optimizing these savings. It is clear that without a strong and viable platform for wellness implementation the projected savings will not be realized. A relatively small change in behavior can pay off with a large return on investment.
VIII. Concluding Remark
The promises of healthcare consumerism can be achieved with expanded use of technology. Technology has supported the infrastructure development, use, and tax advantages of health account balances. New products providing incentives and rewards now use technology to count and credit these financial values. Quality measures, electronic medical records, and provider connectedness are improving with the implementation of technology.
Ultimately, these support technologies for the health system will only be of value if the consumer and patient are engaged. We can not ignore the individual in the disbursement of technology solutions. A successful CDHP program simply can’t afford to forego the opportunities latent in an effective aggregator/navigator front-end: conservative assumptions indicate large paybacks occurring with a year of initial implementation. More liberal, but assumptions could drive even larger net present values. Finally, apart from the direct savings and relatively low risks, the rewards of being a real leader—one genuinely trying to innovate on behalf of plan participants—should be equally compelling.